
Hello, you are using an old browser that's unsafe and no longer supported. Please consider updating your browser to a newer version, or downloading a modern browser.
Hello, you are using an old browser that's unsafe and no longer supported. Please consider updating your browser to a newer version, or downloading a modern browser.
Yes. MMBA is an accredited milk bank that follows strict donor screening, milk processing and dispensing standards established by the Human Milk Banking Association of North America (www.hmbana.org) to ensure the safety of donor human milk. These standards have been established with the advisement of the Centers for Disease Control and Prevention, the US Food and Drug Administration, and the blood and tissue industries. Potential milk donors provide complete medical and lifestyle histories, and undergo blood tests for HIV, HTLV, syphilis, and hepatitis B and C, similar to the screening process used at blood banks. Donated milk is then tested for bacteria and nutritional composition, and pasteurized to kill any bacteria and viruses. Before dispensing, bacteriological testing is repeated to verify that all bacteria are destroyed.
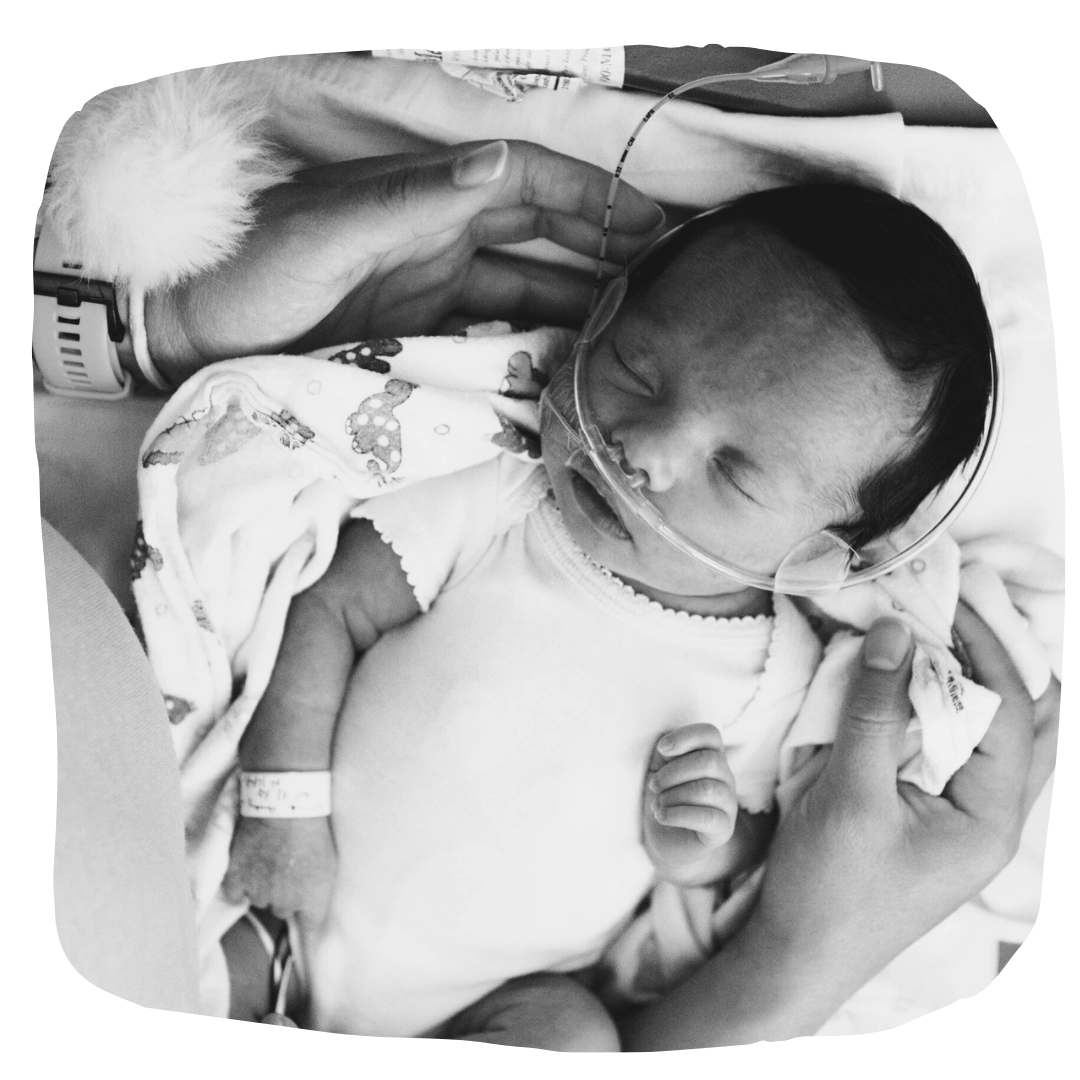
Donor human milk is provided to babies whose mothers do not have their own milk to provide. This situation can happen for a variety of reasons, including: When a mother’s milk supply is delayed due to circumstances of birth or pregnancy, including premature delivery, When a mother’s milk supply does not become established enough to provide sufficient milk for her child or children (twins or triplets, for instance), When stress interferes with milk supply, such as when a hospitalized baby is too at-risk to be held or nursed by their mother, When a mother requires medication that may pass through her own milk and harm her baby, When a mother has a medical condition that makes breastfeeding unsafe, such as HIV.
Donor human milk is dispensed by prescription primarily to babies born premature or who are sick. Common reasons for prescribing donor human milk include preterm birth, especially VLBW or ELBW infants, failure to thrive, malabsorption syndromes, short-gut syndrome, renal failure, inborn errors of metabolism Immunological deficiencies, formula intolerance, cardiac anomalies, gastro-intestinal anomalies, including gastroschisis, intrauterine exposure to drugs
Frozen donated milk is thawed, nutritionally analyzed, cultured for bacteria, pooled for nutrient standardization, and poured into bottles, then pasteurized at 62.5 C in a shaking water bath or automatic pasteurizer. Pasteurized milk is quick-cooled, then frozen at -20’C. Microbiological cultures are obtained by an independent laboratory from individual donors’ deposits prior to pasteurization and pooling, and from each batch of milk after pasteurization. This is done to verify that no heat-resistant pathogens are present before pasteurization, and that there is zero growth of bacteria after the heating process.
Nutritional analysis is conducted at MMBA using a Foss Electric MilkoScan FT120, a full-spectrum infrared spectroscopy, calibrated by us in 2003 to read fat, lactose and protein content of the milk, allowing us to standardize nutrient components of human milk in a process developed in-house called Target Pooling. This standardization allows for strategic feeding of preterm infants, effective evaluation of babies’ growth and development, specific fortification of milk for individual babies, and selection of milk pools that meet individual babies’ needs.
Yes! Research shows that necrotizing enterocolitis (NEC), a primary cause of death and illness for preemies when human milk feedings are unavailable, will increase the medical costs for one baby between $128,000 and $238,000. In addition, reductions in other complications such as retinopathy of prematurity (problems with vision) through the use of donor human milk instead of formula means that the baby goes home sooner with fewer medical issues - and stays healthier long term.
Yes. Mothers’ Milk Bank Austin is one of 30 milk banks who are accredited by the Human Milk Banking Association of North America (HMBANA). HMBANA is an accrediting organization formed in 1985 to promote, protect, and support donor milk banking. It is the only professional membership association for milk banks in Canada and the United States and sets the standards and guidelines for donor milk banking in those areas.

Stories From Moms
Keller’s story moves us every time we watch it. We hope that you can appreciate this beautiful story of a family’s struggles and gratitude.
Stories From Moms
To celebrate 25 years of saving lives through donor milk we decided to turn to Woody Harrison Films once again for his expertise. He had already captured the Memorial...
Stories From Moms
Almost 25 years after Mothers’ Milk Bank at Austin’s founding, we can celebrate our ten millionth ounce of donor human milk dispensed. The Austin Chronicle spoke to Executive Director...
Stories From Moms
No Texan enjoys cold temps and icy roads, but here at Mothers’ Milk Bank at Austin, we don’t let that chilly weather stop us from getting lifesaving donor human...
